Process Improvement in Surgery
- A number of reports supporting the efficacy of process improvement are available. Jimmerson and colleagues, describing results across a broad range of clinical areas at a university-based quarternary medical center, published both general and specific instances of improvement in efficiency and quality. OR processes such as OR turnaround and surgical throughput are fertile areas for such work.
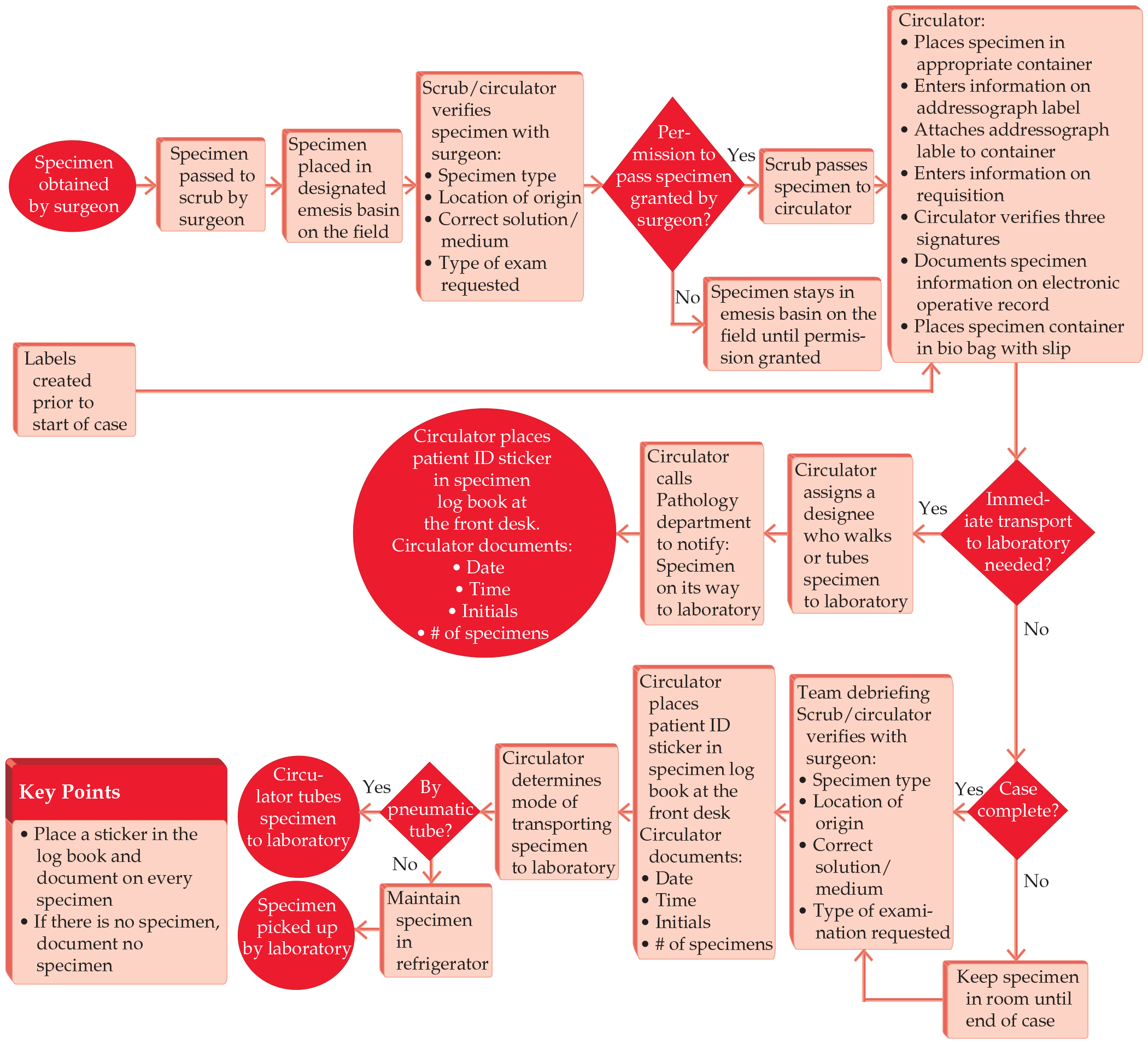
- A core innovation in the origin of “scientific management” was the focus on the details of industrial processes by Frederick W. Taylor. Taylor’s work comes down to us today in the process flow diagram (in TPS Lean terminology, the process flow diagram is referred to as a “value stream map”), which is a schematic representation of the steps in any process, frequently annotated with time intervals and comments.




.png)






