Scientific Foundations: Infection Control in Surgical Practice
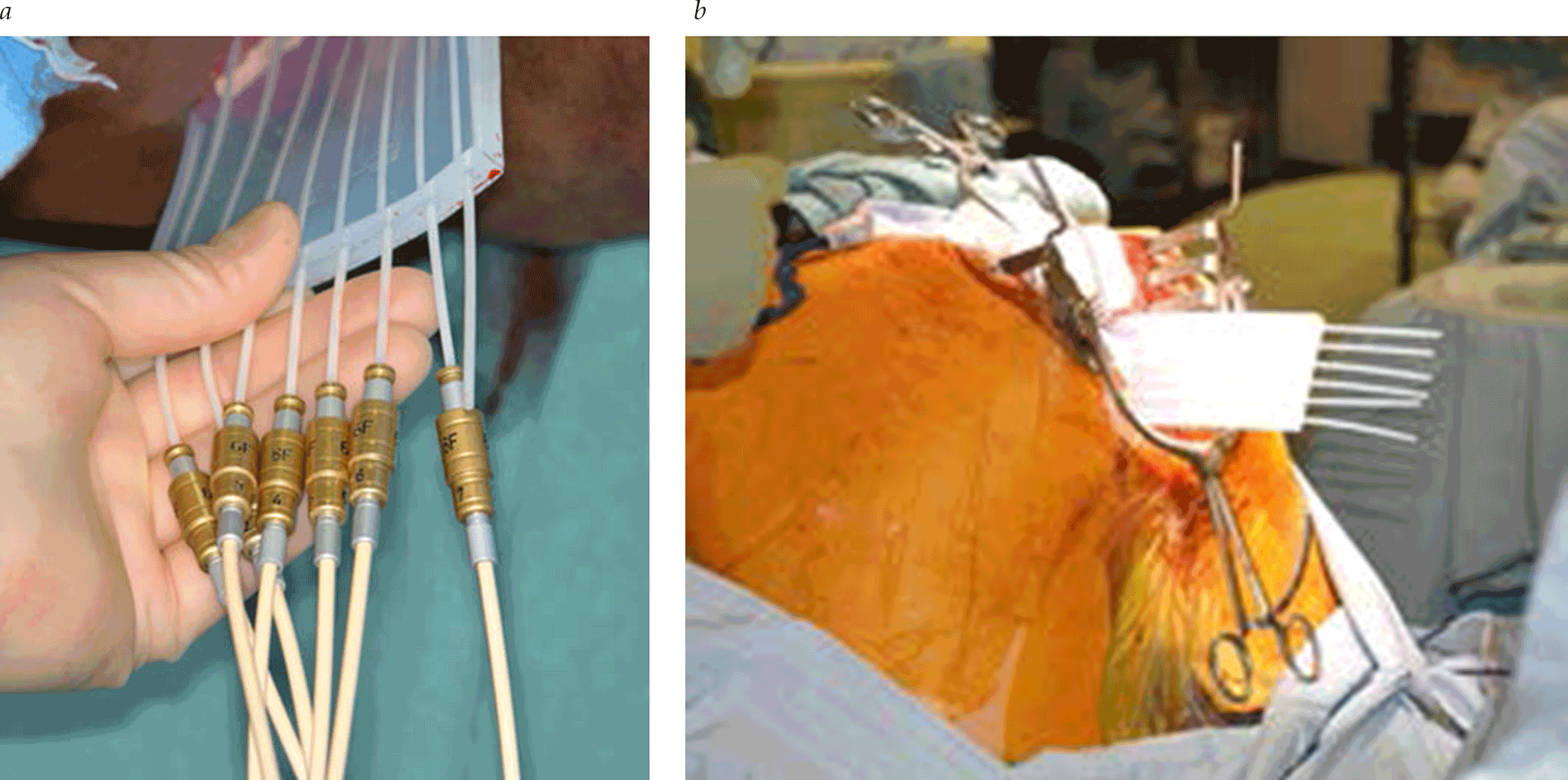
- For patients undergoing surgical procedures requiring the implantation of foreign bodies, colonization with MRSA should be assessed. Hospitalized hemodialysis patients and their health care workers are frequently colonized.
- Updated CDC diagnostic criteria for surgical site infection, catheter-associated urinary tract infection, central line–associated bloodstream infection, and ventilator-associated pneumonia
- Although no single surveillance system captures all HAIs that occur within US acute care hospitals, recent Centers for Disease Control and Prevention (CDC) estimates suggest that 648,000 patients experienced at least one HAI during their hospital stay in 2011. This represents 4.0% of the hospitalized population. Among surgical patients, the rate of reported HAIs is even higher at 10.6%


.png)







