Management and Therapeutic Issues in the Dementias
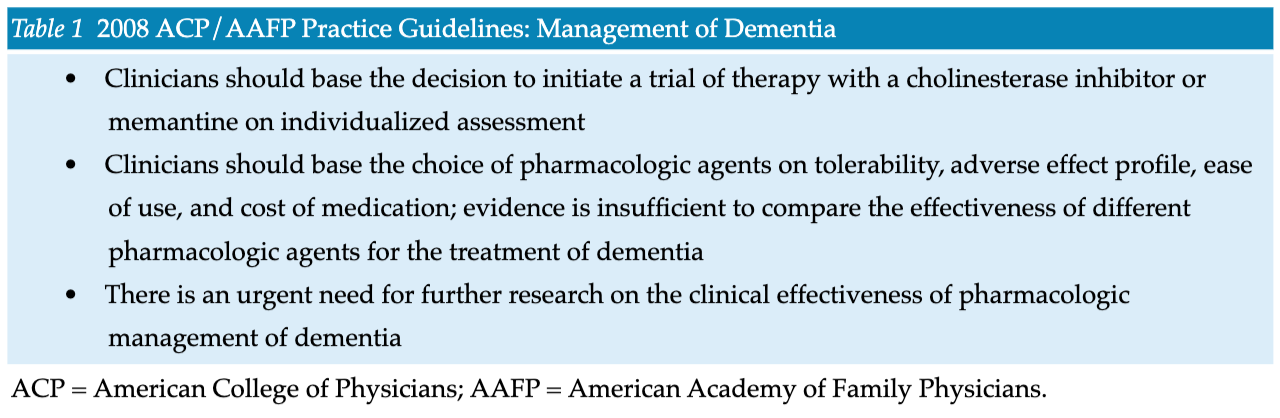
- The cholinesterase inhibitors donepezil, galantamine, and rivastigmine have been approved by the Food and Drug Administration (FDA) for the treatment of AD dementia.
- Patients with mild to moderate AD dementia are the appropriate candidates for cholinesterase inhibitor therapy. These patients need a designated caregiver to supervise the use of the medication.
- Support for and empowerment of the caregivers of dementia patients must be an integral part of management. The emotional and physical health of caregivers is critical to long-term outcomes.


.png)







