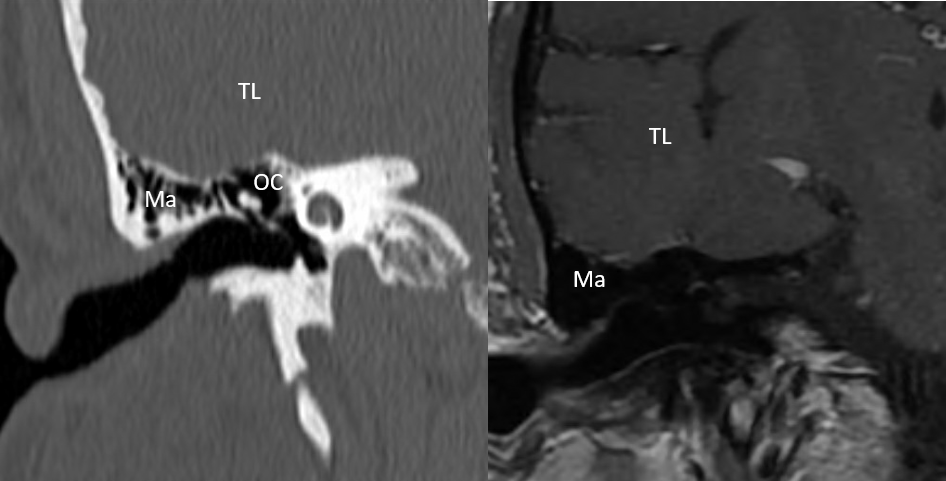
- The proportion of spontaneous CSF leaks is increasing and appears to be related to increasing prevalence of obesity and obstructive sleep apnea
- Resolution of obesity and obstructive sleep apnea may prevent CSF leak recurrence, development of a leak at another site, or even allow a CSF leak to heal without surgery
- Intracranial hypertension is now being recognized as a cause for other otologic and non-otologic symptoms such as headaches and pulsatile tinnitus
Latest Updates
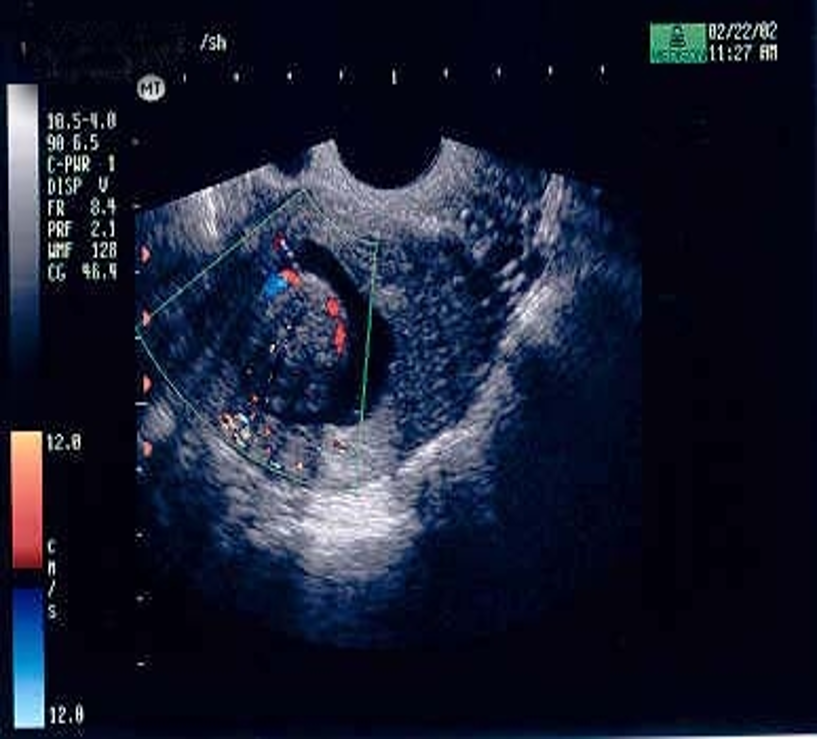
- Zika virus: Delayconception if potential exposure: 8 weeks: females or 3 months: males
- Subclinical hypothyroid: Treatment is associated with improved pregnancy outcomes when TSH levels are above 4 mIU/L.
- Tubal patency: Hysterosalpingo-contrast sonography was recently introduced as an additional screening method to assess tubal patency.
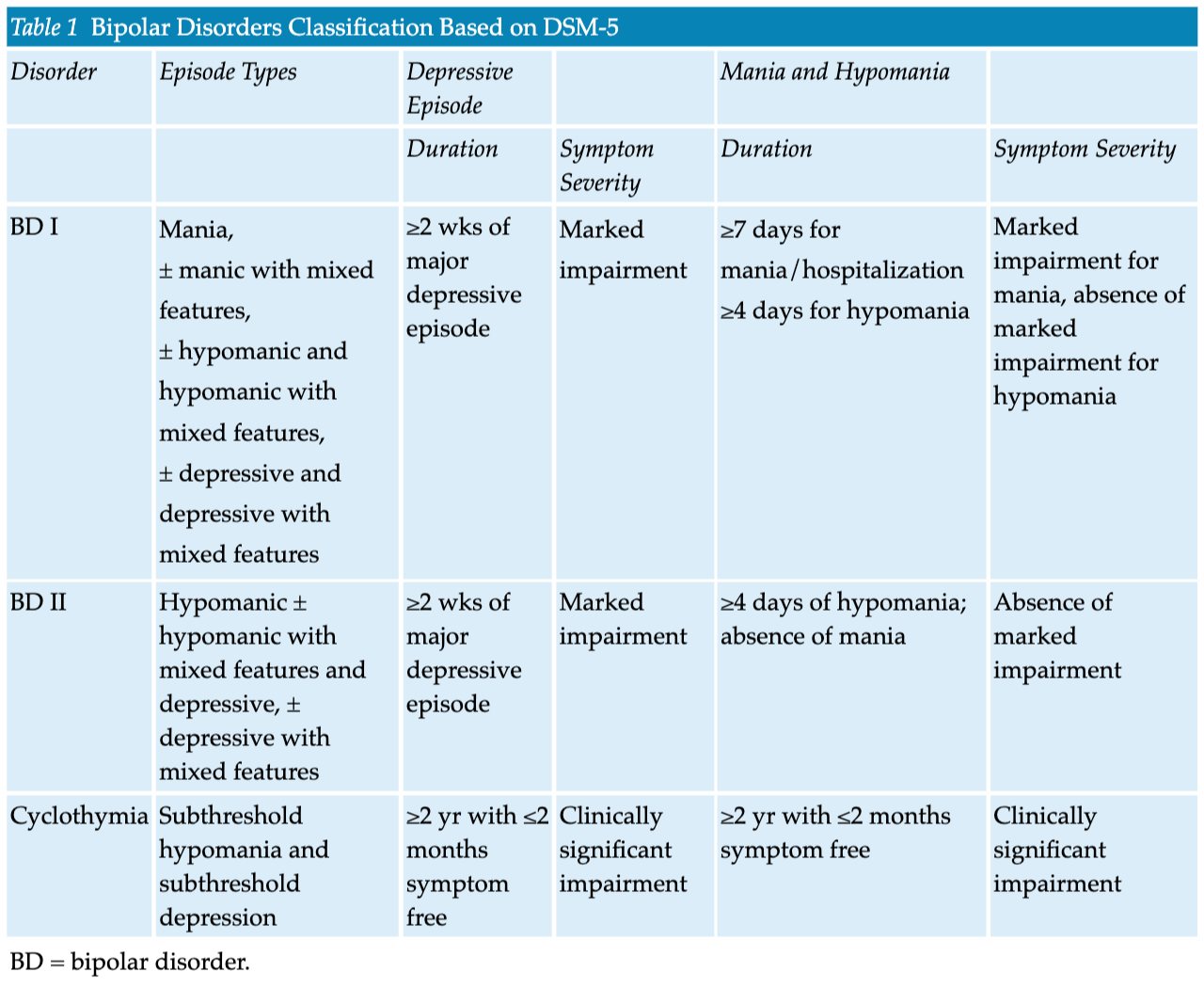
- Review of emerging genetics and etiologic theories of bipolar disorders
- Correlation between recent neurobiologic findings and clinical manifestations of bipolar disorders
- Discussion of the role of endocrine and immune alterations in metabolic derangements associated with bipolar disorders
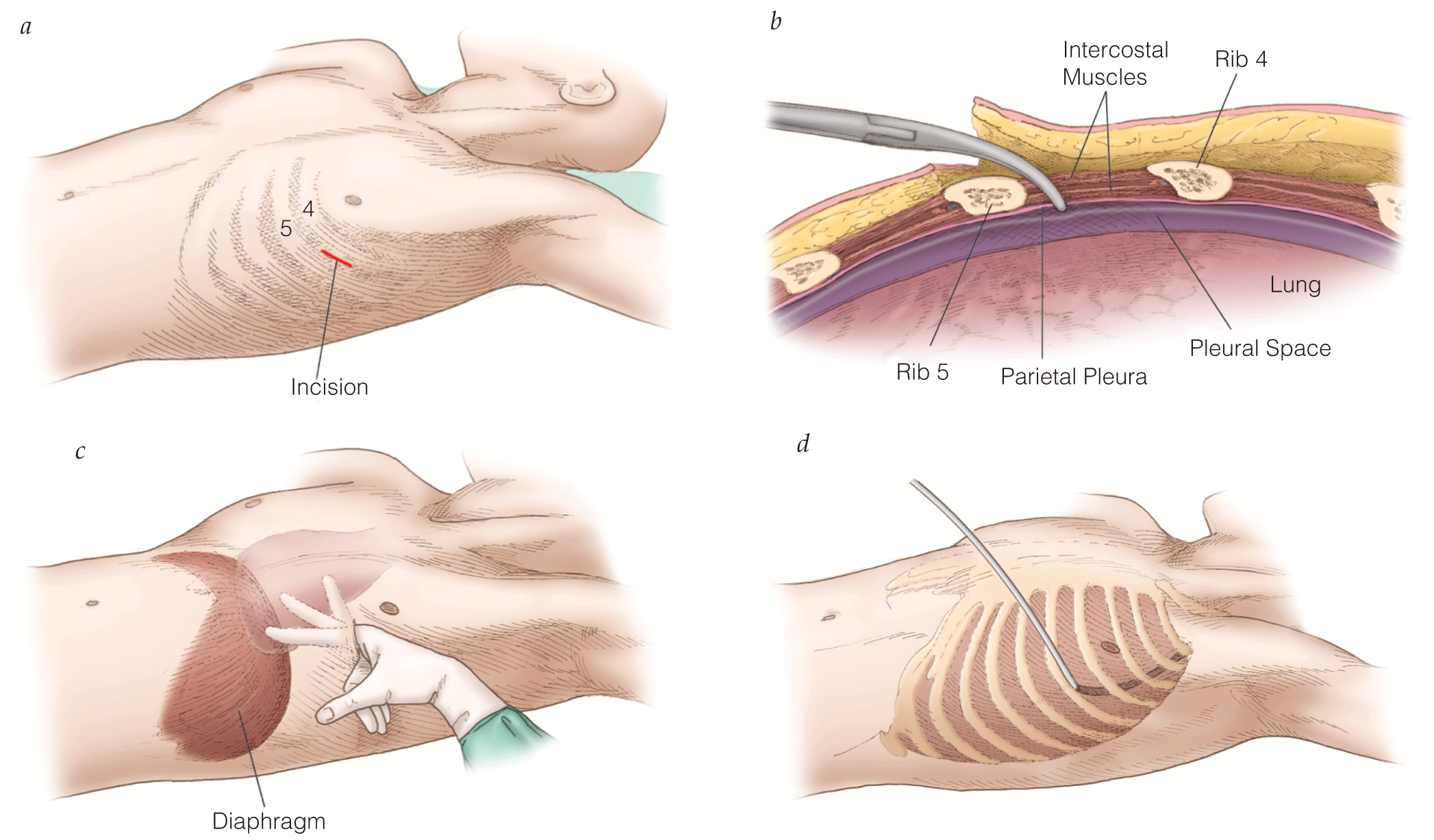
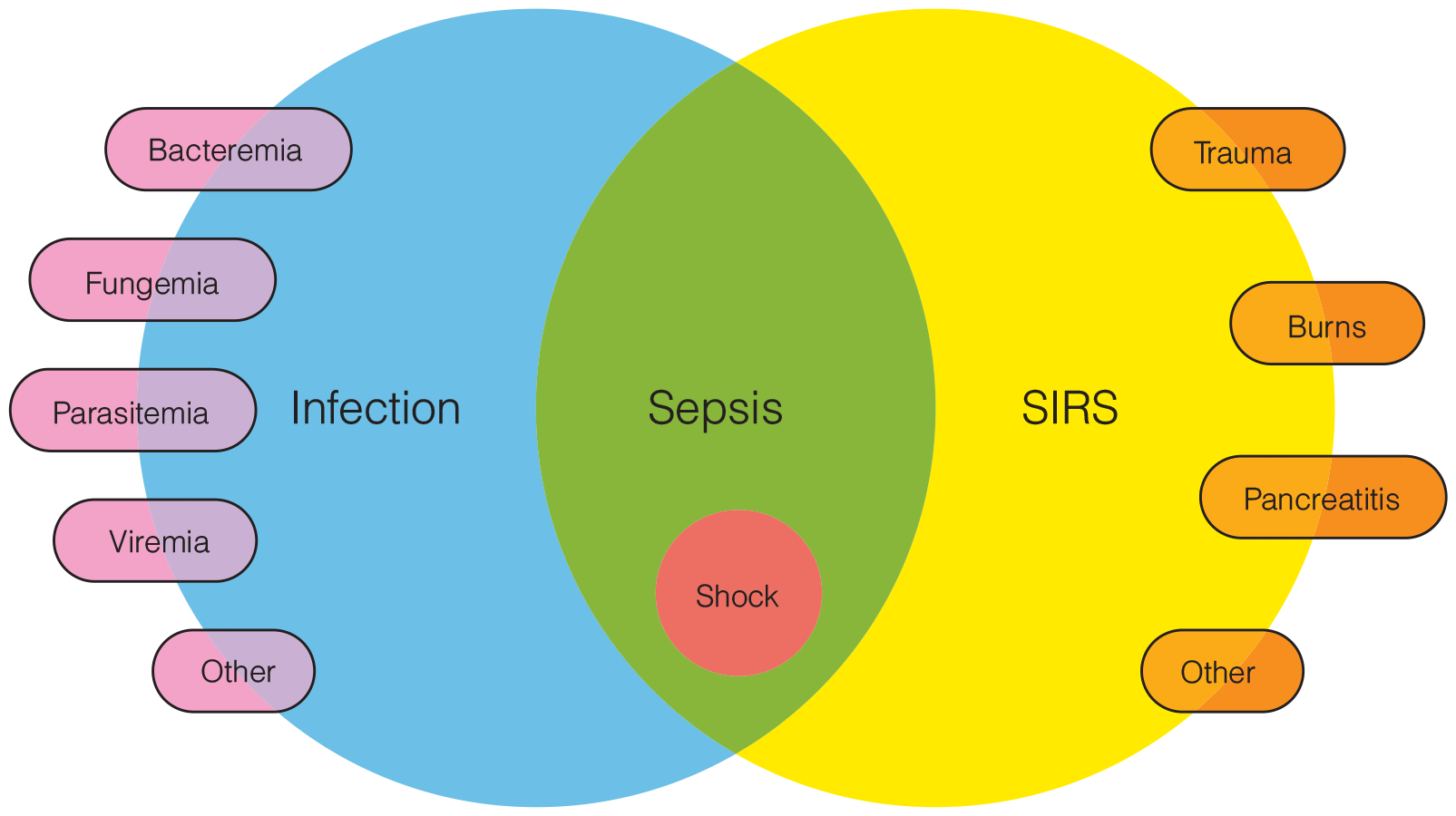
Initial Management of Life-Threatening Trauma
- Initial volume resuscitation should commence with 1 L isotonic crystalloid solution followed by blood products at 1:1:1 ratio (1 unit packed red blood cells to 1 unit fresh frozen plasma to 1 unit platelets) if the patient is not responsive to the initial fluid bolus.
- In patients with massive hemorrhage or evidence of fibrinolysis, tranexamic acid has demonstrated improved survival if administered within 3 hours of injury.
- Use of resuscitative endovascular balloon occlusion of the aorta may be an important adjunct in the control of life-threatening abdominal or pelvic hemorrhage.
- In cases of external hemorrhage of an extremity, a tourniquet should be used to control bleeding.
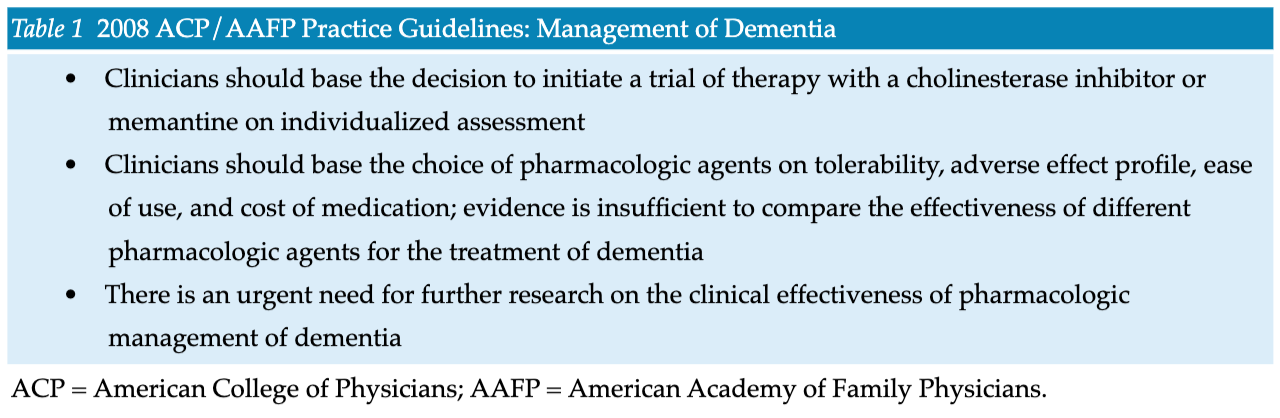
Management and Therapeutic Issues in the Dementias
- The cholinesterase inhibitors donepezil, galantamine, and rivastigmine have been approved by the Food and Drug Administration (FDA) for the treatment of AD dementia.
- Patients with mild to moderate AD dementia are the appropriate candidates for cholinesterase inhibitor therapy. These patients need a designated caregiver to supervise the use of the medication.
- Support for and empowerment of the caregivers of dementia patients must be an integral part of management. The emotional and physical health of caregivers is critical to long-term outcomes.
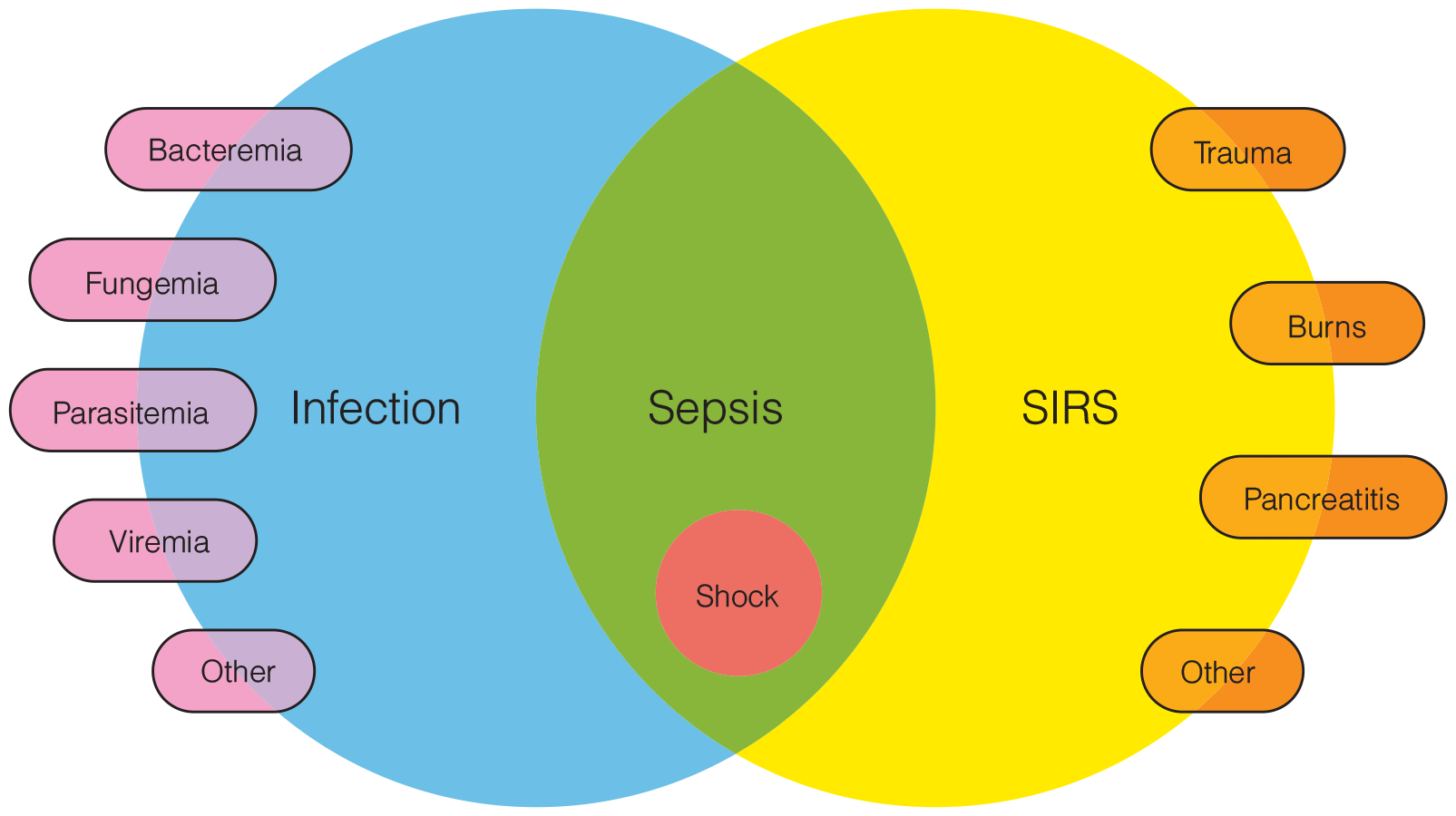
Prevention and Diagnosis of Infection
- Microbiologic studies are critical for characterizing infections. Gram stains and cultures of wound tissue, pus, sputum, urine, and drainage effluent are generally very useful. Identification of not only the particular organism involved but also of its specific antimicrobial susceptibility has become common practice in most hospital clinical laboratories.
- Treatment of CAUTI requires removal or change of the catheter along with systemic antimicrobial therapy. The predominant microorganisms causing CAUTI in the ICU are enteric gram-negative bacilli, Candida species, enterococci, staphylococci, and Pseudomonas aeruginosa. Multidrug resistance is a significant problem in urinary pathogens
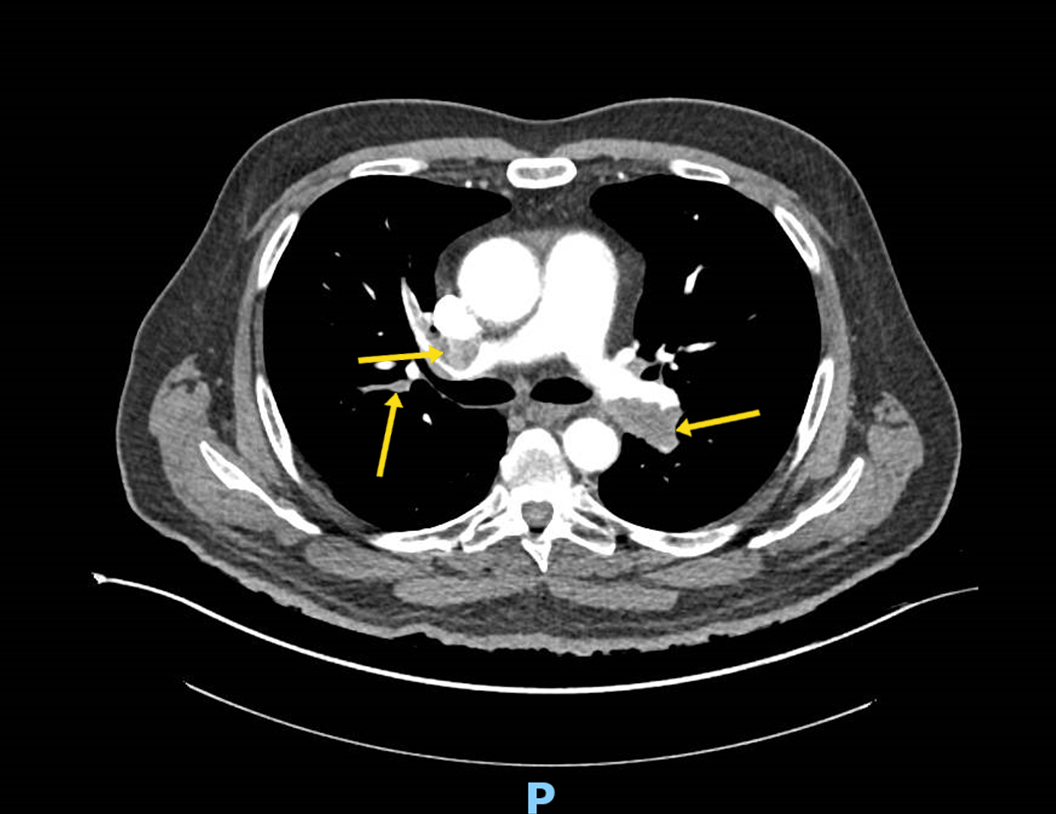
- Clinical gestalt can also accurately assess the pretest probability of PE.
- For patients with a low pretest probability of PE, the Pulmonary Embolism Rule-out Criteria can be used to rule out PE without further testing including no need to order a
- D-dimer.
- The YEARS protocol may be used to exclude a subset of patients from having a workup to rule out PE when their D-dimer is less than 1000 as opposed to 500.
- Novel or new oral anticoagulants are becoming the mainstay of treatment for the hemodynamically stable patient with PE.
- Intravenous alteplase, catheter-directed thrombolysis, surgical embolectomy, and catheter-directed embolectomy are treatment modalities for patients with PE who are hemodynamically unstable.
- For patients in imminent or actual PE-related cardiac arrest, current guidelines recommend a bolus regimen consisting of 50 mg IV t-PA given over two minutes and repeated after 15 minutes in the absence of return of spontaneous circulation.
- A subset of patients with PE can be treated as outpatients if their Simplified Pulmonary Severity Index is 0.
Prevention and Diagnosis of Infection
- Microbiologic studies are critical for characterizing infections. Gram stains and cultures of wound tissue, pus, sputum, urine, and drainage effluent are generally very useful. Identification of not only the particular organism involved but also of its specific antimicrobial susceptibility has become common practice in most hospital clinical laboratories.
- Treatment of CAUTI requires removal or change of the catheter along with systemic antimicrobial therapy. The predominant microorganisms causing CAUTI in the ICU are enteric gram-negative bacilli, Candida species, enterococci, staphylococci, and Pseudomonas aeruginosa. Multidrug resistance is a significant problem in urinary pathogens


.png)







