- Lumbar radiculopathy can cause pain, paresthesia, weakness, reflex changes, and sensory loss and is often isolated to a territory along a specific nerve root. Additionally, symptoms are bilateral in almost 70% of patients. The neurologic examination is often normal in these patients. The straight leg raise (SLR) test has been shown to have a fairly high sensitivity (91%) but low specificity (26%) in detecting lumbar disk herniation.
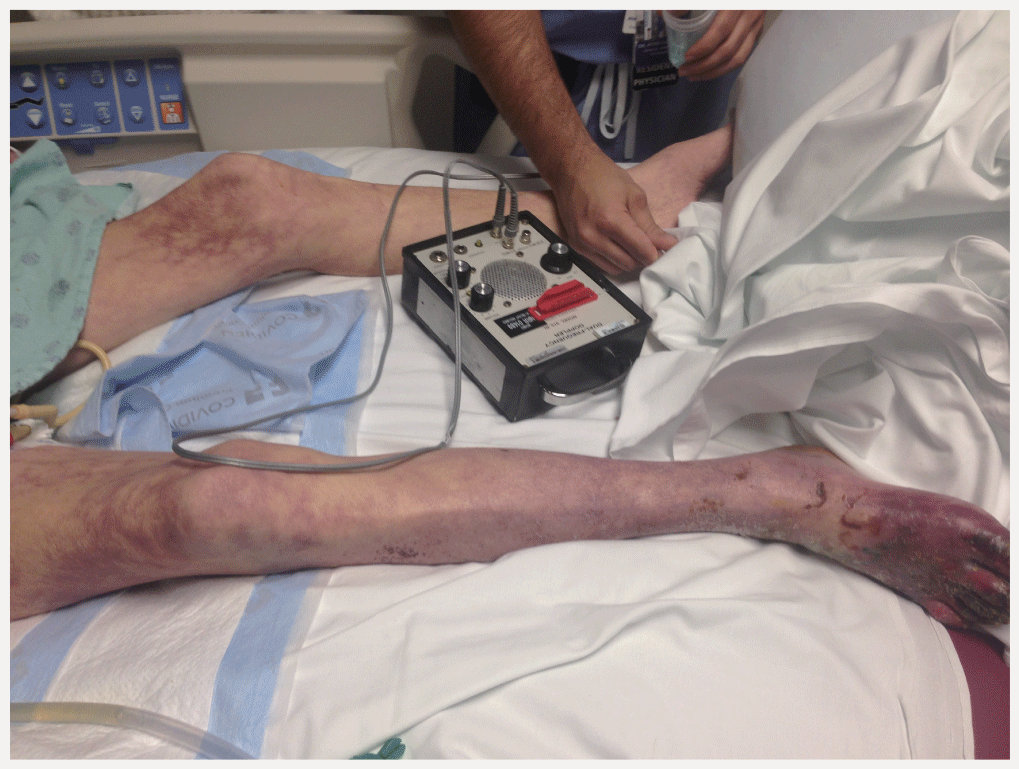
- Computed tomographic angiography (CTA) has increased in popularity for the diagnosis and treatment planning of PAD as the technology has improved. Currently, with 64-slice multidetector imaging, a CTA with runoff can evaluate the chest, abdomen, and legs in a few seconds.
- Surgical intervention is reserved for patients who fail conservative management. Laminectomy is most frequently performed, with favorable results in the absence of spondylolithesis. With the addition of spondylolithesis, fusion is frequently required.
Latest Updates
- Lumbar radiculopathy can cause pain, paresthesia, weakness, reflex changes, and sensory loss and is often isolated to a territory along a specific nerve root. Additionally, symptoms are bilateral in almost 70% of patients. The neurologic examination is often normal in these patients. The straight leg raise (SLR) test has been shown to have a fairly high sensitivity (91%) but low specificity (26%) in detecting lumbar disk herniation.
- Computed tomographic angiography (CTA) has increased in popularity for the diagnosis and treatment planning of PAD as the technology has improved. Currently, with 64-slice multidetector imaging, a CTA with runoff can evaluate the chest, abdomen, and legs in a few seconds.
- Surgical intervention is reserved for patients who fail conservative management. Laminectomy is most frequently performed, with favorable results in the absence of spondylolithesis. With the addition of spondylolithesis, fusion is frequently required.
Medical Management of Pulmonary Arterial Hypertension
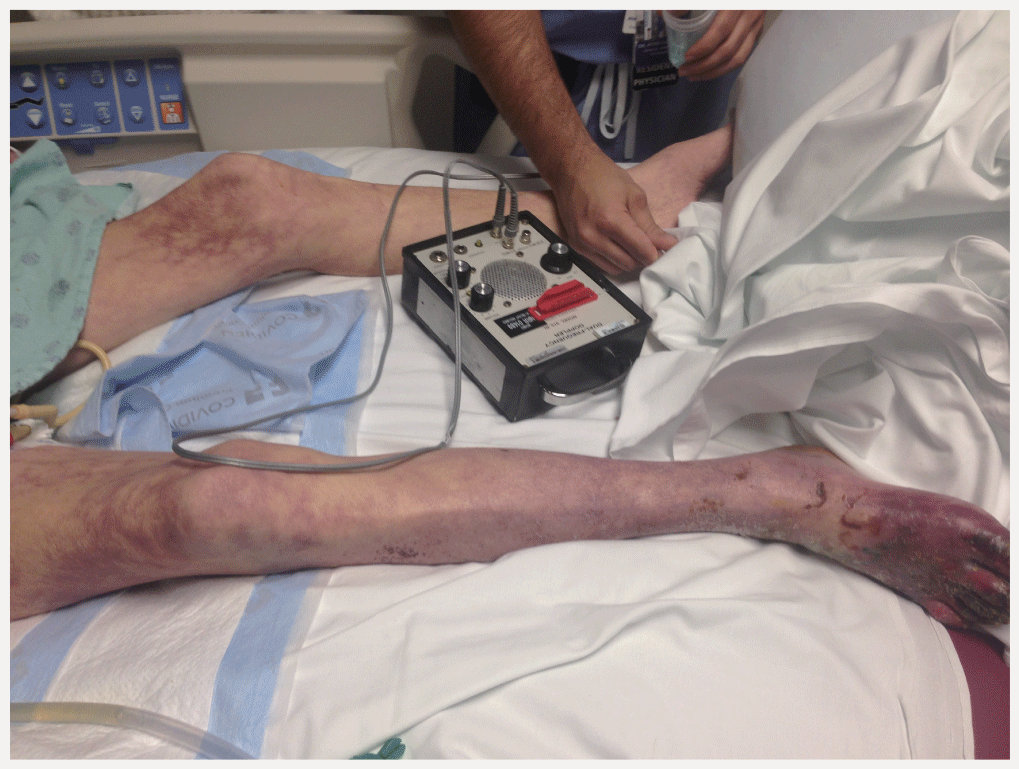
- Over the past two decades, considerable progress has been made in the medical management of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension.
- Recently the field has seen the addition of several new pulmonary vasodilator agents: a soluble guanylate cyclase stimulator (riociguat), a new endothelin receptor antagonist (macitentan) and two new oral prostanoid agents (treprostinil and selexipag).
- Initial combination therapy for the treatment of pulmonary arterial hypertension has heralded a new era in the treatment of PAH. Patients receiving initial combination therapy with a phosphodiesterase inhibitor, tadalafil and an endothelin receptor antagonist, ambrisentan demonstrated improved progression-free survival compared with monotherapy with either tadalafil or ambrisentan.
- For patients with inoperable or persistent chronic thromboembolic pulmonary hypertension, riociguat has emerged as an attractive alternative.

Radiation Wounds and Reconstruction
- Fat grafting presents an emerging strategy to improve tissue quality after radiation-induced fibrosis.
- The author is studying strategies to improve tissue-resident fat content using topical drugs.
- Patient-reported outcomes (PROs) are an important part of research studying the efficacy of strategies against radiation-induced tissue injury.
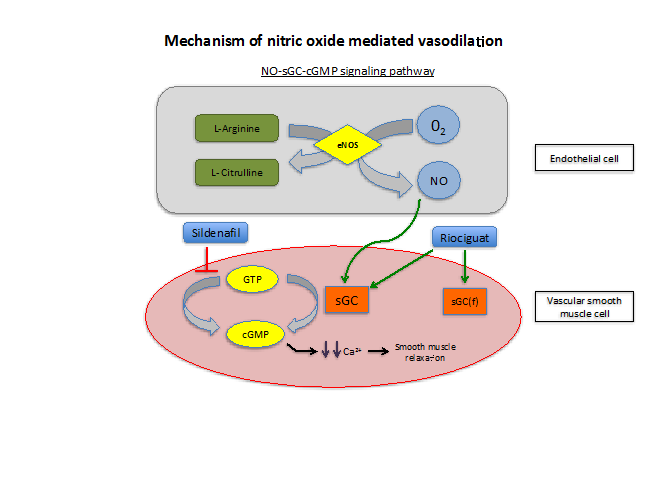
- Angiolytic LASERS such as PDL and KTP lasers target oxyhemoglobin and can eradicate vascular lesions while preserving epithelium.
- Scanners on LASERs allow the LASER beam to create shapes such as lines and semi-circles to optimize efficiency.
- Different modes of energy delivery include ultrapulse and superpulse which allow high peak energy delivery to minimize thermal damage to surrounding tissues.

Surgical Management of Ulcerative Colitis
- As laparoscopic surgery becomes increasingly pervasive, both a hand-assisted and straight laparoscopic colectomy and proctectomy with ileal pouch-anal anastomosis (IPAA) have become more common, with outcomes equivalent to or even improved compared with an open approach.
- Since the introduction of infliximab, biologic therapy has become more prevalent in the inflammatory bowel disease patient population. These medications should be held as long as possible prior to an elective operation as they have been associated with increased infectious complications following IPAA.
- Despite biologic therapy, in the setting of an acute flare of ulcerative colitis, 50% of patients treated with intravenous steroids and an induction done of anti–tumor necrosis factor–α will still go on to have a colectomy within the year.
- The relatively recent introduction of enhanced recovery after surgery protocols in our postoperative care has improved postoperative pain scores and decreased the length of hospital stays. These protocols use a multimodality pain management plan that avoids systemic narcotics, minimizes intravenous fluid administration, enforced early ambulation, and early enteral intake on the night of surgery. The expected length of stay following IPAA is now typically 3 days.
- As an increasing number of immunosuppressive drugs are being introduced for the treatment of ulcerative colitis, a three-stage approach to IPAA is being more commonly employed. A three–stage approach is used for patients who require emergency surgery, are in poor medical condition due to their underlying disease, or are significantly immunosuppressed.

Surgical Management of Ulcerative Colitis
- As laparoscopic surgery becomes increasingly pervasive, both a hand-assisted and straight laparoscopic colectomy and proctectomy with ileal pouch-anal anastomosis (IPAA) have become more common, with outcomes equivalent to or even improved compared with an open approach.
- Since the introduction of infliximab, biologic therapy has become more prevalent in the inflammatory bowel disease patient population. These medications should be held as long as possible prior to an elective operation as they have been associated with increased infectious complications following IPAA.
- Despite biologic therapy, in the setting of an acute flare of ulcerative colitis, 50% of patients treated with intravenous steroids and an induction done of anti–tumor necrosis factor–α will still go on to have a colectomy within the year.
- The relatively recent introduction of enhanced recovery after surgery protocols in our postoperative care has improved postoperative pain scores and decreased the length of hospital stays. These protocols use a multimodality pain management plan that avoids systemic narcotics, minimizes intravenous fluid administration, enforced early ambulation, and early enteral intake on the night of surgery. The expected length of stay following IPAA is now typically 3 days.
- As an increasing number of immunosuppressive drugs are being introduced for the treatment of ulcerative colitis, a three-stage approach to IPAA is being more commonly employed. A three–stage approach is used for patients who require emergency surgery, are in poor medical condition due to their underlying disease, or are significantly immunosuppressed.
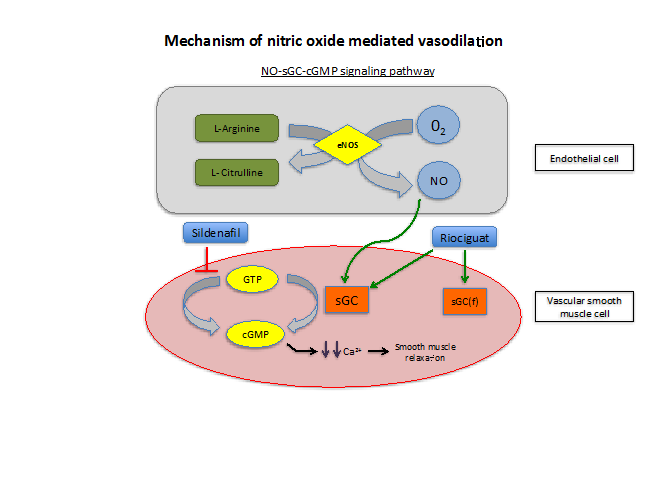
Medical Management of Pulmonary Arterial Hypertension
- Over the past two decades, considerable progress has been made in the medical management of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension.
- Recently the field has seen the addition of several new pulmonary vasodilator agents: a soluble guanylate cyclase stimulator (riociguat), a new endothelin receptor antagonist (macitentan) and two new oral prostanoid agents (treprostinil and selexipag).
- Initial combination therapy for the treatment of pulmonary arterial hypertension has heralded a new era in the treatment of PAH. Patients receiving initial combination therapy with a phosphodiesterase inhibitor, tadalafil and an endothelin receptor antagonist, ambrisentan demonstrated improved progression-free survival compared with monotherapy with either tadalafil or ambrisentan.
- For patients with inoperable or persistent chronic thromboembolic pulmonary hypertension, riociguat has emerged as an attractive alternative.


.png)







